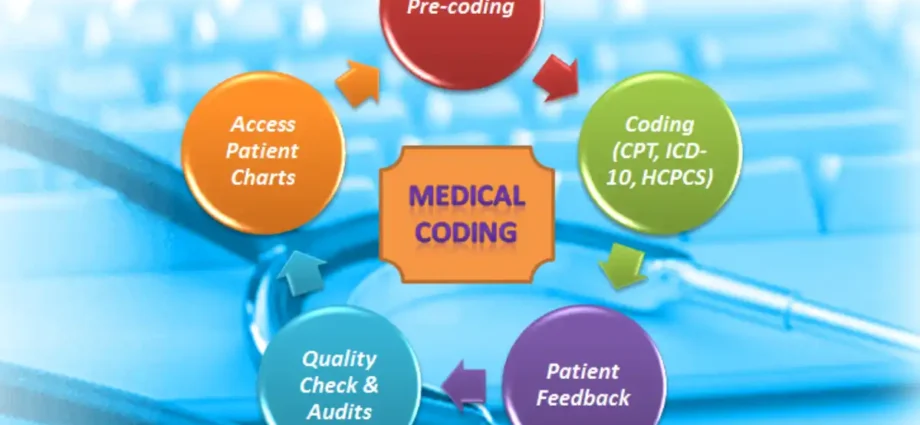
Medical diagnosis, treatments, services, and equipment are all given universal medical alphanumeric codes through the process of medical coding. In this article, We share the details about medical coding, the basics of medical coding, and the uses of medical coding.

What is medical coding?
Medical coding is the process of assigning universal medical alphanumeric numbers to medical diagnoses, treatments, services, and equipment. The diagnosis and procedure codes are located in the medical record paperwork, which also includes transcriptions of doctor’s notes, lab and radiologic data, etc.

Medical coding occurs each time you see a medical expert. The healthcare provider looks over your complaint and medical history, decides on the best course of action after determining the source of your problem, and documents your visit. This documentation provides the basis for the healthcare provider’s remuneration as well as the patient’s permanent record.
The Importance of Medical Coding in the Healthcare Industry
The documentation of decisions, actions, and lessons learned is the foundation of the healthcare income stream. It is necessary to record a patient’s diagnosis, test findings, and course of therapy to ensure future visits will result in high-quality care as well as compensation.
Personal health records are important since they follow a patient through complaints and treatments in the future and need to be easily comprehensible. Given the hundreds of millions of visits, surgeries, and hospital stays that occur in the US each year, this is particularly crucial.
Thousands of ailments, diseases, wounds, and causes of mortality present a problem, though. Providers provide thousands of treatments, and there are an equal number of injectable drugs and supplies that require oversight. These are arranged based on medical codes to make reporting and monitoring easier.

Additionally, each disease, process, and tool in the healthcare industry has its own set of names, acronyms, descriptors, and eponyms. Here, the need for Medical coding comes in the healthcare industry. Medical coding simplifies the presentation and phrasing of these elements, making it simpler to handle, comprehend, and update.
The Health Information Portability and Accountability Act (HIPAA) requires hospitals, providers, and payers to speak in a standard language for ease of communication. Code-dependent, nearly all personal health information is stored on digital media. Digital storage accounts for almost all personal health data, which is code-dependent.
Types of Medical Codes
Medical coding is practiced worldwide, with most countries using the International Classification of Diseases (ICD). The World Health Organization maintains the ICD, and each member nation modifies it to suit its requirements. In the United States, there exist six official code sets defined by HIPAA, each serving a unique function.
ICD-10-CM (International Classification of Diseases, 10th Edition, Clinically Modified)
ICD-10-CM contains codes for anything that has the potential to cause illness, injury, or death. The 69,000 code covers diseases and ailments, neoplasms, toxins, injuries, and activities being done at the time of the injury.
A code, or “smart code,” is a string of up to seven alphanumeric characters that expresses the patient’s complaint in detail. The tracking and medical necessity determination process is carried out using ICD-10-CM. Additionally, it serves as the framework for the MS-DRG system below.
CPT (Current Procedural Terminology)
This collection of approximately 8,000 five-character alphanumeric codes, which identify the services provided to patients by physicians, paraprofessionals, therapists, and other professionals, is owned and maintained by the American Medical Association.
The CPT coding system is used for reporting for most outpatient services. Physicians also utilize it to report services provided in hospitals that accept inpatient patients. This is a glimpse into the CPT code creation process.
ICD-10-PCS (International Classification of Diseases, 10th Edition, Procedural Coding System)

Hospitals employ the 130,000-character ICD-10-PCS code set to define surgical procedures carried out in operating rooms, emergency rooms, and other settings. By approaching ICD-10-PCS coding correctly, you can avoid becoming intimidated by procedural coding.
HCPCS Level II (Health Care Procedural Coding System, Level II)
HCPCS Level II, which consists of more than 7,000 alphanumeric codes, was first developed to enable reporting of procedures and supply billing for Medicare, Medicaid, Blue Cross/Blue Shield, and other providers.

Yet, they’re now employed for a wide range of additional purposes as well, such as assessing quality indicators, charging for outpatient surgery, and academic research. includes other objectives, such as invoicing for outpatient surgery, quality measure monitoring, and scholarly study.
CDT (Code on Dental Procedures and Nomenclature)

The American Dental Association (ADA) is the owner and custodian of CDT codes. The dental portion of HCPCS Level II was once represented by the five-character codes, which begin with the letter D. CDT codes are majorly used for the majority of operations in dentistry and oral health.
NDC (National Drug Codes)
Utilizing a set of codes created by the Federal Drug Administration (FDA), each drug package is monitored and reported. Smart codes with 10–13 alphanumeric characters enable federal agencies, suppliers, and providers to track prescribed, marketed and utilized medications.
Modifiers

CPT and HCPCS Level II codes use hundreds of two-character alphanumeric modifier codes to add further clarity. A change in the service the code represents, a payment instruction, the patient’s condition, the body part being serviced, or a quality component could all be indicated by these codes.
MS-DRG and APC

With the usage of MS-DRG and APCs federal code sets, Payments generated from those systems are made simpler. While indicating the resources used by the facility to carry out the service, they rely on pre-existing code sets.
MS-DRG (Medical Severity Diagnosis Related Groups)

For payment for a patient’s stay, a hospital must record MS-DRGs. The reported ICD-10-CM and ICD-10-PCS codes form the basis of the MS-DRG. A specific set of patient characteristics, such as the primary diagnosis, special secondary diagnoses, procedures, sex, and discharge status, describe them. The Centers for Medicare & Medicaid Services (CMS) and 3M HIS work together to maintain this data set.
APC (Ambulatory Payment Categories)

Through the upkeep of APCs, the Centers for Medicare & Medicaid Services (CMS) supports the Hospital Outpatient Prospective Payment System (OPPS). This system covers payment for certain hospital outpatient services, including minor surgery and other treatments.
Read more: Mpox Outbreak 2024: Indian Health Ministry issues guidelines for airports and hospitals!